Dealing with medical bills can be confusing and stressful. If you or a loved one has received care from Summit Medical Group, you may have questions about how billing and payment works. This comprehensive guide covers everything you need to know about paying your Summit Medical Group medical bills, from payment policies to resolving billing issues.
Overview of Summit Medical Group Billing Process
Summit Medical Group aims to make the billing process as smooth as possible for patients. Here’s a quick overview of how it works:
-
You will receive medical services from Summit Medical Group providers and facilities. This may include primary care, specialists, lab tests, imaging, outpatient procedures, etc.
-
Summit Medical Group will submit a claim to your health insurance company on your behalf
-
Your insurance company will process the claim and send an Explanation of Benefits (EOB) to you explaining what they covered
-
Summit Medical Group will then bill you for any remaining balance based on your plan’s coverage, including copays, deductibles, and any non-covered services.
-
It is your responsibility as the patient to pay the bill or arrange payment plans for any outstanding balances.
When to Expect a Bill from Summit Medical
You typically will not receive a bill immediately after your appointment. It takes time for your insurance company to handle the claim and for Summit to figure out who is responsible.
You can generally expect a bill within 30-60 days of your visit. However, it may take longer if additional claim processing needs to occur.
If you have not received a bill within 60 days, proactively contact Summit Medical Group’s billing department to check the status.
How to Pay Your Summit Medical Bill
You have several options to pay a bill from Summit Medical Group:
-
Online: Pay by credit/debit card or eCheck through the online patient portal.
-
Phone: Call Summit’s billing department at 865-212-3400 and pay over the phone with a card or check info.
-
Mail: Send a check or money order payable to Summit Medical Group to the billing address on your statement.
-
In person: Pay by cash, check, or card at any Summit Medical Group location when you arrive for an appointment.
Always include your patient account number on payments to ensure proper credit to your account.
Payment Plan Options
If you are unable to pay your Summit Medical Group bill in full, you may qualify for a payment plan to split the balance into smaller monthly payments.
To set up a payment plan, contact the billing department and be prepared to provide information about your financial situation. There may be options for:
-
Making fixed monthly payments over 3, 6, or 12 months
-
Paying a percentage of the balance each month
-
Paying a reduced lump sum to settle the account
Discuss the options and come to an agreement on a plan that works within your budget. Get any agreed upon payment plan terms in writing.
What If I Don’t Pay My Bill?
It is important to pay your Summit Medical Group bills in a timely manner or make arrangements if you cannot pay in full. Here is what may happen if a bill goes unpaid:
-
After 90 days without payment, your account is considered delinquent and may be sent to a collections agency.
-
This can negatively impact your credit score if reported.
-
You may no longer be able to schedule non-emergency appointments if your account is in collections.
-
Summit may discharge you as a patient for nonpayment.
Avoid these scenarios by staying communicative with the billing team. Notify them right away if you are unable to make a payment so other options can be discussed.
Am I Required to Pay at the Time of Service?
For most insured patients, payments are not required upfront except for:
-
Copays, which are due when you check in for your appointment
-
Deductibles you still owe for the year
-
Services you are electing to “self-pay” instead of submitting to insurance
If you are uninsured, Summit Medical Group offers self-pay rates and options. Total estimated charges for routine services are provided upfront so you know what to expect to pay at the time of the visit.
More complex services may require a deposit with the balance due after insurance claim processing.
Billing Mistakes and Disputes
If you believe your Summit Medical Group bill is incorrect or shows charges you should not be responsible for, don’t hesitate to speak up.
Some common billing issues that may require investigation include:
-
Being billed for services you did not receive
-
Being charged more than your expected copay/coinsurance amount
-
Receiving duplicate bills for the same service
-
Being billed for non-covered services the provider assured you would be paid by insurance
Contact the billing department about any discrepancies. Provide as much detail as possible about the date/type of service and the issue. Billing staff can review your account details and insurance claims to understand what occurred.
Be persistent and escalate to a manager if needed until the problem is resolved. You have the right not to be responsible for incorrect or disputed charges.
Appeal a Claim Denial or Non-Covered Service
If your insurance company denies a claim that Summit Medical Group submits, you have the right to appeal the decision. Reasons for denials might include:
-
Service deemed “not medically necessary”
-
Out-of-network provider
-
Clinical reason or coding error
-
Missing referral/precertification
Don’t assume you have to pay the provider for denied claims. Begin the appeals process outlined in your Explanation of Benefits (EOB):
-
Request medical records from the provider to support your appeal
-
Submit appeal letters and documents to the insurance company within required timeframes
-
Provide additional clinical notes from your doctor if needed
With persistence, many denials can be overturned. Summit Medical Group billing staff can help point you in the right direction to navigate the process.
Ask Questions Up Front
The best way to avoid billing surprises is to ask questions upfront when scheduling care with Summit Medical Group:
-
Is the provider I’m seeing in my health plan network?
-
Does my insurance require a referral or pre-authorization for these services?
-
What is my copay or coinsurance responsibility for seeing this provider type or having this test?
-
Does my deductible or out-of-pocket max still need to be met?
Your Summit scheduling or billing staff can look up your benefits and provide estimates to help you plan ahead for costs.
Being proactive goes a long way towards a smoother billing experience. Reach out early and often if you have any bill-related concerns.
Price Transparency Tool
Our primary goal at Summit Healthcare is to assist you in making well-informed decisions regarding your healthcare. To access cost estimates for commonly requested medical services, we have designed a user-friendly cost estimator tool. Additionally, our financial counselors are readily available to offer their support and guidance and can be reached at 928-537-6352. For the most precise estimate of out-of-pocket expenses, we recommend reaching out to your insurance provider.
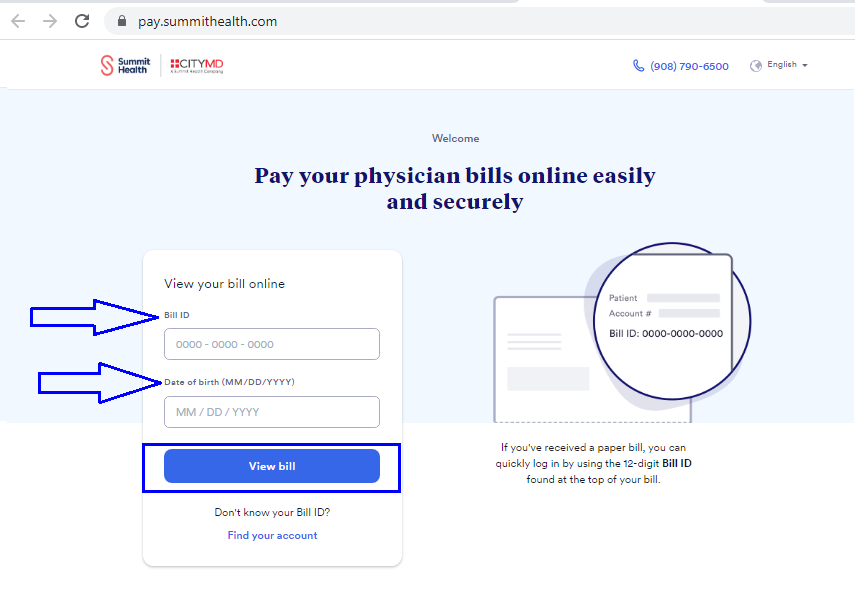
Pay Your Bill Online
Pay a bill after seeing a provider or specialist.
- Answer questions regarding your account
- File your primary and secondary health insurance claims
- Assist you in making a payment
- Provide an itemized bill
