Undergoing a medical procedure can be daunting, and one of the critical aspects is the administration of anesthesia. Anesthesia plays a crucial role in ensuring a safe and comfortable experience during surgery or other invasive procedures. However, the cost of anesthesia services can be a significant concern for many Medicare beneficiaries. In this article, we’ll explore whether Medicare covers anesthetist fees and provide you with a comprehensive understanding of the coverage and associated costs.
Understanding Anesthesia Services
Before delving into Medicare coverage, let’s define what anesthesia services entail. Anesthesia is a medication or combination of medications administered to induce a temporary state of controlled unconsciousness or insensitivity to pain during medical procedures. There are several types of anesthesia, including:
-
Local Anesthesia: This type of anesthesia numbs a specific area of the body and is commonly used for minor procedures such as biopsies or skin treatments.
-
Regional Anesthesia: Regional anesthesia blocks pain in a larger area of the body, such as an arm or leg, and is often used for orthopedic surgeries.
-
General Anesthesia: General anesthesia is a state of controlled unconsciousness, where the patient is completely unaware and insensitive to pain during major surgical procedures.
-
Sedation: Sedation involves administering medications to induce a state of relaxation and drowsiness, but the patient remains conscious and able to respond to verbal commands.
Anesthesia services are typically provided by certified professionals, such as anesthesiologists (physicians specialized in anesthesia) or certified registered nurse anesthetists (CRNAs).
Medicare Coverage for Anesthesia Services
Medicare, the federal health insurance program for people aged 65 and older, as well as certain individuals with disabilities, provides coverage for anesthesia services under specific circumstances. Here’s what you need to know:
Part A (Hospital Insurance) Coverage
If you are an inpatient in a hospital, Medicare Part A covers anesthesia services associated with your hospital stay. This includes anesthesia administered during surgical procedures performed while you are admitted to the hospital.
Part B (Medical Insurance) Coverage
Medicare Part B covers anesthesia services if you are an outpatient in a hospital or receiving treatment at a freestanding ambulatory surgical center. This includes anesthesia for procedures such as colonoscopies, endoscopies, biopsies, and other outpatient surgical services.
It’s important to note that Medicare does not cover anesthesia services for cosmetic procedures or dental anesthesia, except in cases where jaw surgery is required.
Costs Associated with Anesthesia Services under Medicare
Even with Medicare coverage, you may still be responsible for certain out-of-pocket costs related to anesthesia services. Here’s what you can expect:
-
Part B Deductible: Before Medicare starts covering your anesthesia costs, you’ll need to meet the annual Part B deductible, which is $226 in 2023.
-
Coinsurance: After meeting the deductible, you’ll typically pay 20% of the Medicare-approved amount for anesthesia services. Medicare will cover the remaining 80%.
-
Copayments: Some facilities may require you to pay an additional copayment for anesthesia services, which can vary depending on the facility and your specific Medicare plan.
-
Part B Excess Charges: If the anesthesia provider does not accept Medicare’s approved amount as full payment, they may charge you an additional 15% above the Medicare-approved amount. This is known as a Part B excess charge.
To help cover these out-of-pocket costs, many Medicare beneficiaries choose to purchase a Medicare Supplement Insurance (Medigap) plan. Medigap policies can cover some or all of the deductibles, coinsurances, and copayments that Medicare does not cover, including those related to anesthesia services.
Medicare Advantage Plans and Anesthesia Coverage
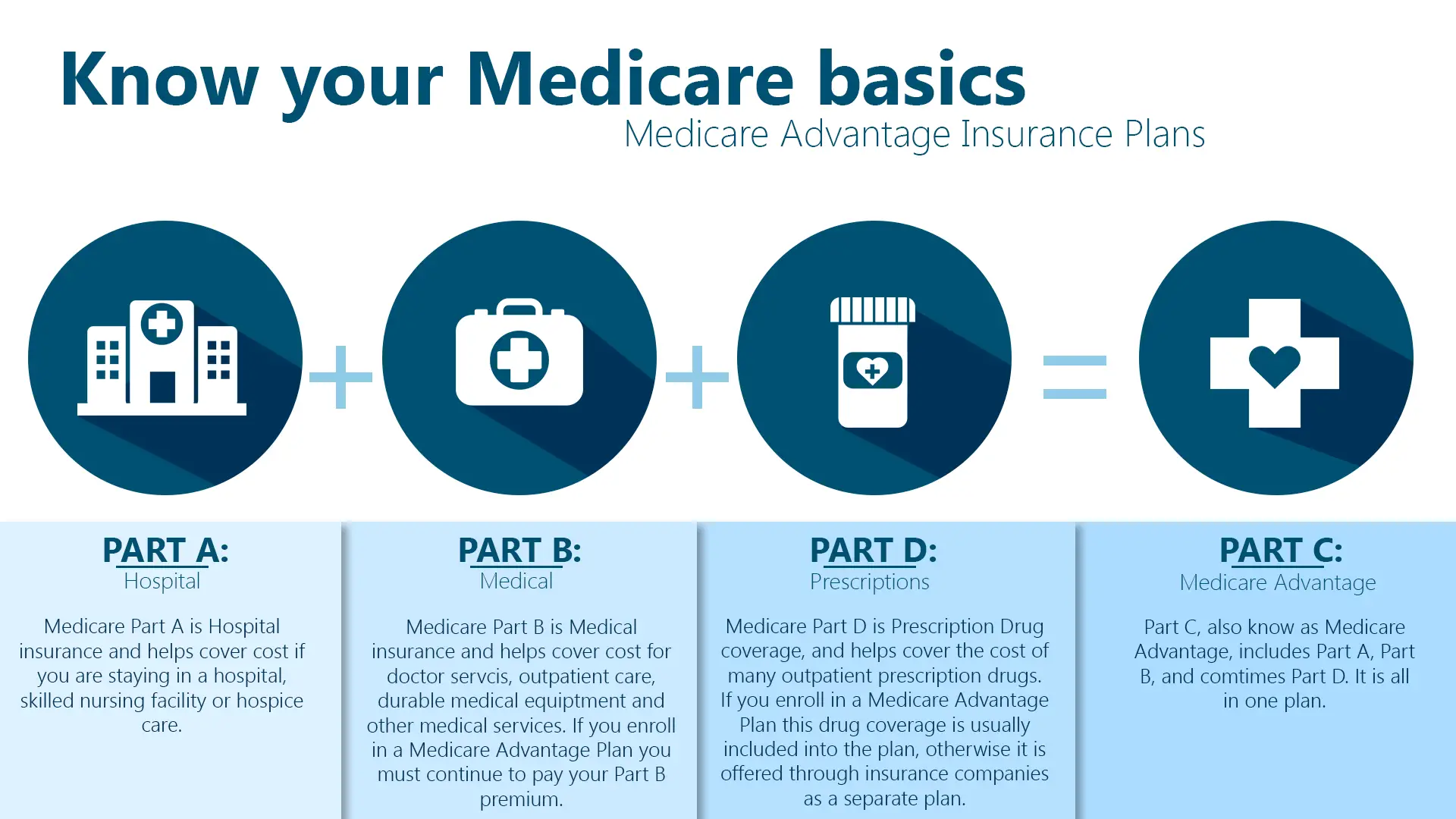
Medicare Advantage plans, also known as Medicare Part C, are offered by private insurance companies and provide an alternative way to receive your Medicare benefits. These plans are required to cover all the services covered by Original Medicare (Parts A and B), including anesthesia services.
However, Medicare Advantage plans may have different cost-sharing structures, such as copayments or coinsurance, and may require you to use in-network providers to receive full coverage for anesthesia services. It’s essential to review your specific Medicare Advantage plan details to understand the coverage and costs associated with anesthesia services.
Tips for Minimizing Anesthesia Costs with Medicare
While Medicare provides coverage for anesthesia services, there are steps you can take to minimize your out-of-pocket expenses:
-
Choose providers who accept Medicare assignment: Providers who accept Medicare assignment agree to charge no more than the Medicare-approved amount, eliminating the risk of Part B excess charges.
-
Consider a Medigap plan: As mentioned earlier, a Medicare Supplement Insurance (Medigap) plan can help cover the deductibles, coinsurances, and copayments that Medicare does not cover, including those related to anesthesia services.
-
Explore Medicare Advantage plans: Compare the costs and coverage of different Medicare Advantage plans in your area to find one that best suits your needs and budget for anesthesia services.
-
Plan ahead: If you know you will be undergoing a procedure that requires anesthesia, discuss the costs with your healthcare provider and plan accordingly to minimize any surprises.
Conclusion
Medicare provides coverage for anesthesia services associated with inpatient hospital stays (Part A) and outpatient procedures (Part B), but beneficiaries may still be responsible for deductibles, coinsurances, and copayments. Understanding your coverage options and exploring supplemental insurance plans can help you manage the costs of anesthesia services effectively. By being an informed Medicare beneficiary, you can ensure a safe and comfortable experience during your medical procedures while minimizing financial strain.
Will Medicare Cover My Procedure? | Everything You Need to Know
FAQ
Does Medicare pay for anesthesia services?
How much does Medicare pay for anesthesia for colonoscopy?
How is anesthesiologist billed?
Can a facility bill for anesthesia?