Are you curious about whether Medicare Part A covers lab work? As you navigate the complexities of Medicare coverage, it’s essential to understand what services are covered under each part. In this comprehensive guide, we’ll dive deep into the details of Medicare Part A and its coverage for lab work, ensuring you have the information you need to make informed decisions about your healthcare.
Understanding Medicare Part A
Medicare Part A is the hospital insurance component of Original Medicare. This part covers inpatient hospital stays, skilled nursing facility care, hospice care, and some home health care services. It’s important to note that Part A is generally premium-free for most beneficiaries, as long as they or their spouse paid Medicare taxes while working.
What Lab Work Does Medicare Part A Cover?
When it comes to lab work, Medicare Part A provides coverage for certain diagnostic tests and procedures performed during an inpatient hospital stay or skilled nursing facility stay covered by Part A. Here are some examples of lab work covered under Medicare Part A:
- Blood Tests: Various blood tests ordered by your doctor during a covered inpatient stay, such as complete blood counts (CBCs), basic metabolic panels, and blood chemistry tests.
- Urine Tests: Urinalysis and other urine tests that may be necessary during your hospital or skilled nursing facility stay.
- Tissue Samples: If your doctor orders a biopsy or tissue sample analysis during your covered inpatient stay, Medicare Part A will typically cover the associated lab work.
- Diagnostic Imaging: Certain diagnostic imaging tests, such as X-rays, CT scans, and MRI scans, may be covered by Part A if ordered during your inpatient stay.
It’s important to note that Medicare Part A coverage for lab work is limited to tests and procedures performed during a covered inpatient stay. If you require lab work on an outpatient basis, such as routine blood work or diagnostic tests at a lab or doctor’s office, those services would generally be covered under Medicare Part B.
Understanding Costs and Coverage Limitations
While Medicare Part A covers a significant portion of lab work during inpatient stays, there are some costs and limitations to be aware of:
- Deductible: For inpatient hospital stays covered by Part A, you’ll be responsible for paying the annual deductible, which is $1,600 in 2023.
- Coinsurance: After the deductible is met, you may be responsible for coinsurance payments for extended hospital stays beyond 60 days.
- Coverage Limitations: Medicare Part A coverage is limited to medically necessary services and lab work ordered by your doctor during your inpatient stay. Any additional tests or procedures not deemed medically necessary may not be covered.
It’s essential to understand these costs and coverage limitations to plan and budget accordingly for your healthcare expenses.
Maximize Your Coverage with Medicare Part B
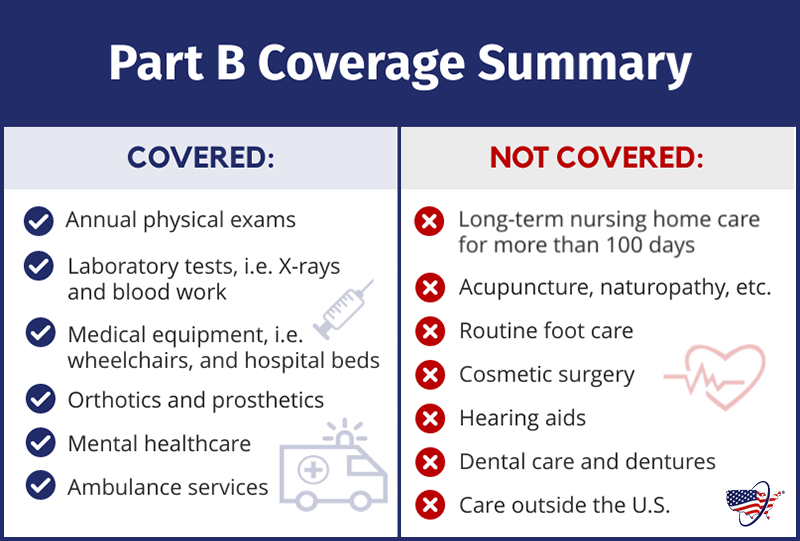
While Medicare Part A covers lab work during inpatient stays, many beneficiaries also enroll in Medicare Part B to receive comprehensive coverage for outpatient services, including lab work. Part B covers a wide range of diagnostic tests, such as:
- Blood tests
- Urinalysis
- Fecal occult blood tests
- Pap tests
- Prostate-specific antigen tests
With Part B, you’ll typically pay a 20% coinsurance after meeting the annual deductible for these outpatient lab services. Additionally, Part B covers preventive screenings like cardiovascular disease screenings and certain cancer screenings, which can help detect and address health issues early on.
Conclusion
Medicare Part A provides essential coverage for lab work performed during inpatient hospital stays and skilled nursing facility stays covered by Part A. However, it’s important to understand the costs and limitations associated with this coverage. For comprehensive lab work coverage, many beneficiaries opt for a combination of Medicare Part A and Part B, ensuring they have access to both inpatient and outpatient lab services. By understanding the nuances of Medicare coverage, you can make informed decisions about your healthcare and plan accordingly for any out-of-pocket expenses.
How Medicare Covers Blood Tests
FAQ
Does Medicare Part A cover diagnostic tests?
Is routine bloodwork covered by Medicare?
What does the Medicare Part A cover?
What lab tests are not covered by Medicare?